 ...the monthly, Open Access Publisher.
...the monthly, Open Access Publisher.
 ...the monthly, Open Access Publisher.
...the monthly, Open Access Publisher.
Research Article - (2023) Volume 10, Issue 1
Received: 08-Mar-2023, Manuscript No. AJMSOA-23-91123; Editor assigned: 10-Mar-2023, Pre QC No. AJMSOA-23-91123 (PQ); Reviewed: 24-Mar-2023, QC No. AJMSOA-23-91123; Revised: 08-May-2023, Manuscript No. AJMSOA-23-91123 (R); Published: 16-May-2023
Background: Informed consent is the process of communication between a patient and health care provider that results in the patient’s authorization/agreement to undergo a specific medical/surgical intervention. The practice of surgical informed consent among health care providers was considered as poor and the health care workers did not meet the minimum standards yet when they conducted informed consent with patients.
Objective: This study was aimed to assess practice and factors associated with informed consent process for major surgical procedures among health care workers in Wachemo university, Nigist Eleni Mohamed Memorial comprehensive specialized hospital, Hosanna Southern Ethiopia. 2022.
Method: Institutional based cross sectional study was conducted among 422 health care workers from 9 August to 21, 2022. Each study units were selected based on the proportionally allocated sample size from each profession by simple random sampling method; self-administered pretested questionnaire was used to collect all necessary data. Then data was, entered into epi data version 3.1, exported to statistical package for social science version 25 for cleaning and analysis. The bivariate logistic regression model was used to explore factors associated with surgical informed consent practice, variables with p-value of <0.25 became candidates for final model (multivariable logistic regression model). Then finally, odds ratio with 95% confidence interval and p-value of <0.005 was used to identify variables which were significantly associated with dependent variable.
Results: A total of 422 sample size with 98.1% response rate, of which 223 (53.9% (CI; 48.3-58.4) had good surgical informed consent practice. Being age between 31-35 years (AOR=2.392; 95% CI: 1.33-14.467), no language barrier in communication with patients (AOR=2.011; 95% CI: 1.848-8.511), availability of policy/regulation that support surgical informed consent process (AOR=3.201; 95% CI: 1.102-9.298), spending more time 21-30 minutes on consent process (AOR=5.006; 95% CI: 1.659-15.100), patients with history of previous surgery (AOR=3.141; 95% CI: (1.435-6.876), having good knowledge (AOR=3.931; 95% CI: 1.799-8.591) and favorable attitude (AOR=5.690; 95% CI: 2.729-11.862) were significantly and positively associated with good informed consent practice.
Conclusion: The surgical informed consent practice is still inadequate for globally recommended standard among the health care workers at the comprehensive University Hospital and more emphasis and work up need for quality health service.
•Since practice need more observational study and thisstudy was cross sectional, it lacks proven validity andmore robust evidence on practice of SIC process.
•As the study was conducted in a single referral hospital,even though it’s a tertiary health facility it could notgeneralizable for the health care workers in other healthfacility that are usually below the level of this institutionas a whole.
•Self-reporting bias might also affect the outcome of thestudy, since some respondents may not report what theyactually practice.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
All related data have been presented within the manuscript. The data set supporting the conclusion of this article can be obtained from the corresponding author upon reasonable request.
Our grateful thank goes to Bahir Dar university, college of medicine and health science, department of Midwifery for giving us this golden and educative opportunity. We would also like to extend our deepest gratitude to WCU-NEMM comprehensive specialized hospital management and medical staff for providing us with the necessary information.
Last, but not least we would like to express our special gratitude to the data collectors, supervisors study participants and all who helped and supported us during this work.
TTW*, BAA, FWS, EA, and AN contributed to the conception, designed the study, supervised the data, carried out the analysis, interpreted the data, and revised the work for important intellectual content. TTW and BAA participated in framing the method and wrote the manuscript for publication. All authors read and approved the final manuscript.
Ethical clearance approval was obtained from the Institutional Review Bord of Bahir Dar university (IRB-CMHS), college of medicine, and health sciences. Before the actual data collection started, permissions letter was obtained from the study hospital. During the distribution of questionnaires, informed consent was taken from study participants and information was provided about the purpose and the benefit of the study along with their full right to refuse or completely reject to participation in the study. Considering their safety, explanation of the potential risk towards taking their time during interview and informing that no incentives or other benefits are given to participate in the study. Finally, all eligible health care workers were allowed to involve in the interview and confidentiality or privacy of information was maintained.
Authors declare that they have no conflicts of interest.
During the distribution of questionnaires, informed consent was taken from study participants and information was provided about the purpose and the benefit of the study along with their full right to refuse or completely reject to participation in the study. Considering their safety, explanation of the potential risk towards taking their time during interview and informing that no incentives or other benefits are given to participate in the study. Finally, all eligible health care workers were allowed to involve in the interview and confidentiality or privacy of information was maintained.
Ethical clearance approval was obtained from the Institutional Review Bord of Bahir Dar university (IRB-CMHS), college of medicine, and health sciences before the actual data collection started, permissions letter was secured from the study hospital.
Health-care workers, Major surgeries, surgical informed consent, Practice, Quality health service
•Since similar studies were very rare so far in ourcountry, therefore this study tried to show index ofpractice of SIC for major surgical procedures amongHCWs in my context, and being a base line for futureresearchers.
•This study addressed new variables (pts’ related factors)which significantly associated.
53.9% of health care workers had good surgical informed consent practice which is inadequate for globally (WHO) recommended standard that stated as, all patients have right to be informed participants of any medical or surgical procedures happening to their body. Patient with previous history of surgery, when both patient and patient relatives sign SIC form, age, language, working experience, time spent for the consenting process availability of policy/regulation that supports process of SIC in the institution, Knowledge, attitude of the health care workers had a statistically significant positive association with the surgical informed consent practice.
Even if the finding of SIC practice in this study was 53.9% but still, it is low for quality service and looks as it is theoretical ideal, which needs more emphasis and work up. Therefore, it is suggested that, Similar study should be done on different public and private hospitals to compare the result to know which hospital health professionals have had better SIC practice from public and private sectors in the area, Supervision manual on SIC should be developed that could be applied to monitor the health professional’s performance, The hospital also should avail the standardized policy/regulation drafts in the institution that regulates work of every health care professional in the hospital and find away all professionals aware of it, further studies/ preferably observational study should be done to assess SIC professionals for improved validity and more robust evidence on SIC.
This study, founds 223 (53.9%; CI:48.3-58.4) of HCWs had good SIC practice, this finding was in agreement with the study done in Ethiopia, bale zone hospitals 50.01%. But is higher than study done in Uganda and SPHMMC Addis Ababa that were 48% and 8.1% respectively. The variation might be due to that, this study was carried out at a single study area where the study participants unfortunately might share similar features. However, it is lower result as compared to those studies done at Sat tam bin Abdul-Aziz university Al-Kharj city (Saudi Arabia) and Brazil where 69.7% and 59.6%, HCWs had good SIC practice respectively. This might be due to events like Saudi Arabia and Brazil are countries with middle per capital income thus, their health care system varies from our country (sub-Saharan Africa) where demands and supply (health care system, workforce particularly, surgeons) were further disproportionate in which one surgeon might obligated to treat so many patients, that can affect the quality of SIC practice. Or might be due to the different data collection method, an online questionnaire based data collection method used in Saudi Arabia, the small sample size (133) and regression models (Back ward LR) used in Uganda. The justification is further supported by evidence found in WHO data 2000–2007, where on average, across sub-Saharan Africa, a population of 10,000 is served by two doctors and 11 nursing and midwifery personnel, compared to 32 and 79 respectively serving the same number of people in Europe.
In this study, only 13.8% of the respondents always obtain informed consent from patients for major surgical procedures. This is very low than the finding in similar study conducted in our country bale zone where 55.2% of HCWs always obtains SIC for major surgeries. The discrepancy might be that, lack of formally documented policy/regulation that clearly supports SIC process in the institution, this is supported by the finding in this study, where majority 256 (61.8%) of the study participants do not know if the hospital had policy/regulation that supports SIC process.
Regarding factors associated with SIC practice, odds of good SIC practice for the HCWs who were in age group of 31-35 years were 2.4 times higher than those who were in age group of 21-25 years, this finding was congruent with the study conducted in Ethiopia bale zone and Aga Khan university hospital, Karachi, Pakistan. This could be explained as age increases, their work experience increases, increasing exposure to training and shared experience as a result, HCWs increase their knowledge and attitude, leading to improved SIC practice.
In this study, health care workers who never faced challenge in communication with their patients due to language barrier were 2 times more likely had good SIC practice than their counter parts, this finding is similar with the finding in the study conducted at Aga Khan university hospital, Karachi, Pakistan. Possible explanation for this could be that, when there is shared language between patients and their health care providers it results in common understanding among them that lead HCWs to have good SIC practice.
HCWs that spent more time (21-30 minutes) on providing information about SIC process to their surgical patients were 5 times more likely to have good SIC practice than those HCWs who spent five minutes and less time. This finding is similar to study done in Ethiopia bale zone and Addis Ababa. The rational for this might be that, taking more time in providing information to patients gives the patient more time space to ask more questions on their doubts and provide both the HCWs and patients with wider discussion period which finally leads to have common understandings and shared decision and results HCWs in good SIC practice.
This study revealed that, HCWs who were aware of availability of policy/regulation that supports SIC process in the hospital had 3.2 times higher odds of good SIC practice than those who do not know if institution has policy/regulation that supports SIC process. The finding is in line with the study done in our country bale zone, hospitals. Justification for this might be that, when there is regular supervision and control of activity in working environment from the higher officials according the available policy/regulation, the employee’s commitment and effectiveness of work implementation increases. This is supported by findings from study done in USA which shows, mid level managerial involvement/supervision influences effective implementation of work.
This study also found that, there is a significant association between good SIC practice among HCWs and treating surgical patients with history of previous surgery, based on the finding, odds of good SIC practice for health care workers were 3 times higher when they treated patients with history of previous surgery is higher than when they treated neither of patients with no previous surgical history nor patients with previous history of repeated surgery, it is congruent with finding in the study done at Jima University medical center, and Hawassa university, referral hospital southern Ethiopia, shows a significant association between patients previous exposure to surgery and easily signing of SIC in recent schedules. Possible reason might be due to preoperative health education of patients in their previous surgery and the patients already experienced the reality of surgical treatment.
In this study, the health care workers who had well SIC knowledge were 3.9 times more likely to practice adequate SIC than those who had poor knowledge. This finding was similar with the study conducted in bale zone Ethiopia, which might know the informed consenting process helps integrate each component of consent into practice quickly and thoughtfully. It is a fact that without the basic understanding of the elements of the consenting process, the approach of informed consent will not be optimal. Similarly, those HCWs with favorable attitudes toward SIC were 5.69 times more likely to practice adequate informed consent than those with unfavorable attitudes. This finding is comparable with the study in bale zone Ethiopia and Pakistan. The possible explanation might be that a favorable attitude towards informed consent practice is fundamental and enhances motivation for practice.
Socio-demographic characteristics of the respondents
A total of 422 sample size, with 98.1% successful response rate. The respondents’ mean age was 29 years (SD; ± 5.244), ranging from 21 to 52 years. Almost half, 215 (51.9%) were Females and more than half, 238 (57.5%) were Orthodox Christians, about 213 (51.4%) were nurses, 209 (50.5%) of the respondents had 5 years and less working experience and more than half 259 (62.6%), had faced a challenge in communication with their patients easily due to language barriers (Table 1).
| Variables | Frequency | Percent (%) | |
|---|---|---|---|
| Age group (years) | 21-25 | 130 | 31.4 |
| 26-30 years | 121 | 29.2 | |
| 31-35 years | 98 | 23.7 | |
| >35 years | 65 | 15.7 | |
| Male | 199 | 48.1 | |
| Sex | Female | 215 | 51.9 |
| Orthodox | 238 | 57.5 | |
| Religion | Protestant | 127 | 30.7 |
| Muslim | 43 | 10.4 | |
| Others* | 6 | 1.4 | |
| Nurse | 213 | 51.4 | |
| Professional status | Midwives | 71 | 17.2 |
| Anesthesia | 41 | 9.9 | |
| Physicians | 64 | 15.5 | |
| Others** | 25 | 6 | |
| Work experience (years) | </=5 yrs. | 209 | 50.5 |
| 6-10 years | 152 | 36.7 | |
| >10 years | 53 | 12.8 | |
| Communication challenges (Language barrier) | Yes | 259 | 62.6 |
| No | 155 | 37.4 | |
Note: **Diploma nurse; Midwives and PHO; *Apostolic religion
Table 1. Socio-demographic characteristic of participants in the study of practice and factors associated with surgical informed consent process among health care workers in WCU-NEMMCS hospital, hosanna southern Ethiopia, 2022. N=414.
Organizational related characteristics of the respondents
Out of the total participants, 256 (61.8%) reported that they do not know if the institution has policy or regulation that supports the practice of SIC, 189 (45.7%) of them reported, the contents of the informed consent form is adequate to obtain valid consent, only 19 (4.6%) of the participants had attended in service training on the SIC process, and almost all 403 (97.3%) reported that they had no administrative support (like interpreters available) in their institution. 178 (43.0%) of the participants had provided care for more than 10 patients in an average per shift, and nearly one fourth 94 (22.7%) spends 5-10 minutes on providing information to their patients about the procedure during their professional encounter (Table 2).
| Variable | Frequency | Percent (%) | |
|---|---|---|---|
| Adequate content of informed consent | Yes | 189 | 45.7 |
| No | 73 | 17.6 | |
| Don’t know | 152 | 36.7 | |
| Training attended on informed consent (in service training) | Yes | 19 | 4.6 |
| No | 395 | 95.4 | |
| Policy/regulation in institution | Yes | 98 | 23.7 |
| No | 60 | 14.5 | |
| Don’t know | 256 | 61.8 | |
| Administrative support | Yes | 11 | 2.7 |
| No | 403 | 97.3 | |
| Average number of patients cared per shift | <5 | 103 | 24.9 |
| 6-10 | 133 | 32.1 | |
| >10 | 178 | 43 | |
| Time spent for consenting process (in minutes) | <5 | 93 | 22.5 |
| 6-10 | 94 | 22.7 | |
| 11-20 | 67 | 16.2 | |
| 21-30 | 70 | 16.9 | |
| >30 | 90 | 21.7 | |
Table 2. Organizational related characteristic of participants in the study of practice and factors associated with surgical informed consent process among health care workers in WCU-NEMMCS-Hospital, hosanna southern Ethiopia, 2022. N=414.
Patients related characteristics of the respondents
Of the total participants, 279 (67.4%) of them reported that, they have faced surgical patients refused to sign SIC during their professional carriers, almost half 209 (50.5%) of them think the reason behind the patients refuse to sign the SIC was anxiety and fear of surgery. 156 (37.7%) of the study participants responded that patients and patient relatives are responsible persons to sign the SIC, and when asked about if they ever faced any patient influenced by someone else to sign SIC, about 192 (46.4%) responded they have never faced any surgical patient influenced by someone else to sign the SIC, 217 (52.4%) participants reported that surgical patients with history of repeated surgery are more easily cooperative to sign the SIC (Table 3).
| Variables | Frequency | Percent (%) | |
|---|---|---|---|
| Have you ever faced patient’s refuses to sign SIC form? | Yes | 279 | 67.4 |
| No | 135 | 32.6 | |
| What do you think the reason for the patients to refuse? | Lack of knowledge on sic | 130 | 31.4 |
| Anxiety and fear of surgery | 209 | 50.5 | |
| Others** | 75 | 18.1 | |
| Which patients are usually refuses to sign on the SIC form? | Patients scheduled for elective surgery | 80 | 19.3 |
| Patients scheduled for emergency surgery | 235 | 56.8 | |
| Don't know | 99 | 23.9 | |
| Who usually signs on the SIC form | The patient themselves | 144 | 34.8 |
| Pts and relatives | 156 | 37.7 | |
| Relatives | 114 | 27.5 | |
| Have you ever faced patients influenced by someone else | Often | 91 | 22 |
| Sometimes | 131 | 31.6 | |
| Never | 192 | 46.4 | |
| Have you ever faced a patient with history of repeated surgery? | Yes | 276 | 66.7 |
| No | 138 | 33.3 | |
| Which patients are easily cooperative to sign SIC form?
|
Patients with no previous history of surgery | 84 | 20.5 |
| Patients with history of previous surgery | 217 | 52.4 | |
| Don’t know | 113 | 27.3 | |
Table 3. Patient’s related characteristic of participants in the study of practice and factors associated with surgical informed consent process among health care workers in WCU-NEMMCS hospital, hosanna southern Ethiopia, 2022. N=414.
Knowledge and attitude of health care workers on the SIC
The mean score of study participants’ knowledge was 15.615, and more than half, 227 (54.8% CI; 49.9-58.7), HCWs had good Knowledge on SIC (Figure 2). The mean score of study participants’ attitude was 35.6, and similarly, more than half, 226 (54.6% CI; 49.1-59.4), HCWs had favorable attitude towards the SIC.
Practice of surgical informed consent process
Out of the total participants, less than quarter, 57 (13.8%), of participants reported that, they always obtained informed consent for major surgical procedures, only 109 (26.3%) informed the reason/indication for surgery and nearly 1/4th, 134 (32.4%) of the study participants reported that, they always inform the patients about type of anesthesia to be used. Less than half, 110 (26.6%), always informed the patients about the presence/absence of treatment options similarly, less than one third, 119 (28.7%), reported they always discussed the risk/potential complications of the procedure to their surgical patients. 1/4th, 107 l(25.8%) of participants discussed the presence of any favorable environment and the possibility to say no to the proposed surgery, and nearly, 2/3rd 177 (42.8%) had checked that their patients understood the explanations they provided to them (Table 4).
The mean score of study participants’ SIC practice was 26.9976, and almost half, 223(53.9% (CI; 48.3-58.4) of the HCWs had good SIC practice.
| Items | Response | ||
|---|---|---|---|
| Never | Sometime | Always | |
| N (%) | N (%) | N (%) | |
| I obtain informed consent from patients for major surgical procedures | 68 (16.4) | 289 (69.8) | 57 (13.8) |
| I inform the patients why the surgery will be performed | 75 (18.1) | 230 (55.6) | 109 (26.3) |
| I inform the patients about presence/absence of alternative treatment option/s to surgery | 98 (23.7) | 206 (49.8) | 110 (26.6) |
| I inform the patients about type of anesthesia to be used | 213 (51.4) | 67 (16.2) | 134 (32.4) |
| I explain the benefit of the procedure to the patient | 78 (18.8) | 210 (50.7) | 126 (30.4) |
| I explain the risks or potential complication/s related to the procedure to the patient | 100 (24.2) | 195 (47.1) | 119 (28.7) |
| I explain favorable environment to say no to the proposed surgery | 145 (35) | 162 (39.1) | 107 (25.8) |
| I inform the patients about consequences of refusing the proposed surgery | 83 (20) | 200 (48.3) | 131 (31.6) |
| I provide counseling aids including the recommended treatment which assist in decision making to the patients | 136 (32.9) | 171 (41.3) | 107 (25.8) |
| I provide adequate time for decision to sign on the informed consent form | 48 (11.6) | 266 (64.3) | 100 (24.2) |
| I provide an opportunity to ask questions to the patients | 40 (9.7) | 252 (60.9) | 122 (29.5) |
| I assess the competence of my patients to give consent to treatment/procedure | 20 (4.8) | 214 (51.7) | 180 (43.5) |
| I check that my patients understand the explanations I provided to them | 18 (4.3) | 219 (52.9) | 177 (42.8) |
Note: N represents frequency.
Table 4. Practice of participants in the study of practice and factors associated with surgical informed consent process among health care workers in WCU-NEMMCS hospital, hosanna southern Ethiopia, 2022. N=414.
Factors associated with surgical informed consent practice
In the bivariate analysis, variables male sex, categorical age 26-30 and 31-35 years, working experience above 10 years, no language barrier for communication with patients, number of patients seen per day/shift, Time spent 21-30 and >30 minutes to provide information on SIC-process to the patients, adequate content of consent form (standardized format), presence of policy/regulations in the institution, on site training, patients scheduled for emergency surgery, when both the patients and relatives sign the SIC, when patients were not influenced by relatives/someone else to sign SIC, patients with history of previous surgery, good knowledge and favorable attitude of health care workers, showed a p-value of <0.25 and became candidates for multivariable analysis. In multivariable binary logistic regression, categorical age 31-35 years, no challenges in communication with patients due to language barrier, time spent, 21-30 minutes to provide information on SIC process to thesurgical patients, availability of policy/regulation that supportsSIC process, patients with history of previous surgery, goodknowledge and favorable attitude of HCWs were statistically,and positively associated with good SIC-practice of the healthcare workers at a p-value< 0.05.
Odds of good SIC practice for the health care workers in agegroup of 31-35 years were nearly 2.4 times higher than thoseHCWs who were in the age group of 21-25 years (AOR=2.392;95% CI: 1.330-14.467). And HCWs workers who never facedchallenge in communication with their patients due to languagebarrier were almost 2 times more likely to have good SIC-practice, when compared to those who faced challenge incommunication with their patients due to language barrier(AOR=2.011; 95% CI: 1.848-8.511).
Health care workers who spent 21-30 minutes to provideinformation on SIC to their surgical patients were 5 times hadgood SIC-practice compared to those who spent a time of less than 5 minutes to provide information on SIC to their patients (AOR=5.006; 95% CI: 1.659-15.100) and HCWs who were aware of availability of policy or regulation that supports SIC practice in the institution were 3.2 times had good SIC practice than, those who do not aware of whether there is policy/regulation or not in the institution that supports SIC practice (AOR=3.201; 95% CI: 1.102-9.298). Likewise, odds of good SIC practice were 3 times higher when they treated surgical patients with history of previous surgery than when they never treated neither of surgical patients with history of previous surgery nor patients with no previous history of surgery (AOR=3.141; 95% CI: (1.435-6.876).
Furthermore, HCWs who have good SIC knowledge were 3.9 times likely to have had good SIC practice when compared to those who have poor SIC knowledge (AOR=3.931; 95% CI: 1.799-8.591) and at last but not least, HCWs with favorable attitude towards SIC were 5.69 times had good SIC practice than those with unfavorable attitude towards SIC (AOR=5.690; 95% CI: 2.729-11.862) (Table 5).
| Variables | Practice of SIC | Binary logistic regression | Multivariable logistic regression | |||
|---|---|---|---|---|---|---|
| Good N (%) | Poor N (%) | COR (95% CI) | P-value | AOR (95% CI) | ||
| Age group in years | 21-25 | 40 (30.8) | 90 (69.2) | 1 | ||
| 26-30 | 79 (65.3) | 42 (34.7) | 4.232 | 0.353 | 3.003 (2.550-18.685) | |
| 31-35 | 61 (62.2) | 37 (37.7) | 3.709 | 0.011 | 2.392 (1.330-14.467)* | |
| >35 | 43 (66.2) | 22 (33.8) | 4.398 | 0.023 | 2.289 (0.472-11.088) | |
| Sex of the participants | Male | 135 (67.8) | 64 (32.2) | 3.044 | 0.172 | 1.038 (0.516-2.090) |
| Female | 88 (40.9) | 127 (59.1) | 1 | |||
| Work experience in years | ≤5 | 84 (40.2) | 125 (59.8) | 1 | ||
| 6-10 | 103 (67.8) | 49 (32.2) | 3.128 | 0.033 | 2.306 (0.859-6.159) | |
| >10 | 36 (67.9) | 17 (32.1) | 3.151 | 0.028 | 4.173 (0.857-20.312) | |
| Faced communication challenges with pats due to Language barrier | Yes | 115 (44.4) | 144 (55.6) | I | ||
| No | 108 (69.7) | 47 (30.3) | 2.877 | 0 | 2.011 (1.848-8.511)* | |
| Time spent on SIC process. | <5 | 39 (39.4) | 60 (60.6) | 1 | ||
| 6-10 | 53 (46.6) | 61 (53.5) | 0.984 | 0.957 | 0.563 (0.204-1.551) | |
| 11-20 | 48 (60.8) | 31 (39.2) | 2.242 | 0.314 | 1.498 (0.540-4.153) | |
| 21-30 | 32 (68.1) | 15 (31.9) | 6.136 | 0.003 | 5.006 (1.659-15.100) ** | |
| >30 | 51 (68.0) | 24 (32.0) | 5 | 0.031 | 2.013 (0.736-5.506) | |
| Adequate content of consent form | Yes | 108 (57.1) | 81 (42.8) | 2.161 | 0.001 | 1.324 (0.619-2.829) |
| No | 57 (78.1) | 16 (21.9) | 5.774 | 0.042 | 1.506 (0.466-4.870) | |
| Don’t know | 58 (38.2) | 94 (61.8) | 1 | |||
| Policy regulations support SIC? | Yes | 85 (86.7) | 13 (13.3) | 9.556 | 0 | 2.846 (1.081-7.491)* |
| No | 34 (56.7) | 26 (43.3) | 1.911 | 0.025 | 0.504 (0.181-1.404) | |
| Don’t know | 104 (40.6) | 152 (59.4) | 1 | |||
| Had training on the SIC practice? | Yes | 16 (84.2) | 3 (15.8) | 4.844 | 0.013 | 0.684 (0.086-5.428) |
| No | 207 (52.4) | 188 (47.6) | 1 | |||
| Which patients usually refuses to sign on the SIC form? | Elective | 33 (41.3) | 47 (58.1) | 1.177 | 0.597 | 0.767 (0.265-2.215) |
| Emergency | 153 (65.1) | 82 (34.9) | 3.127 | 0 | 1.442 (0.548-3.794) | |
| Don’t know | 37 (37.4) | 62 (62.6) | 1 | |||
| Who usually signs SIC? | Patients only | 73 (50.7) | 71 (49.3) | 2.321 | 0.241 | 2.004 (1.162-5.838) |
| Pts and relatives | 115 (73.7) | 41 (26.3) | 6.331 | 0.013 | 4.194 (3.849-21.961) | |
| Relatives only | 35 (30.7) | 79 (69.3) | 1 | |||
| Faced pts influenced by relatives to sign SIC? | Often | 29 (31.9) | 62 (68.1) | 1 | ||
| Sometimes | 62 (47.3) | 69 (52.7) | 1.921 | 0.022 | 1.656 (0.515-5.322) | |
| Never | 132 (68.8) | 60 (31.3) | 4.703 | 0 | 1.776 (0.553-5.704) | |
| Faced a patient with previous surgical history? | Yes | 170 (61.6) | 106 (38.4) | 2.572 | 0 | 1.085 (0.418-2.82) |
| No | 53 (38.4) | 85 (61.6) | 1 | |||
| Which pts easily give SIC? | With no Hx | 13 (15.5) | 71 (84.5) | 0.298 | 0.031 | 0.237 (0.083-0.679) |
| With history | 167 (77) | 50 (23.0) | 5.437 | 0.013 | 3.141 (1.435-6.876)** | |
| Don’t know | 43 (38.1) | 70 (61.9) | 1 | |||
| Knowledge | Good | 161 (70.9) | 66 (29.1) | 4.918 | 0 | 3.931 (1.799-8.591)** |
| Poor | 62 (33.2) | 125 (66.8) | 1 | |||
| Attitude | Favorable | 167 (73.9) | 59 (26.1) | 6.672 | 0 | 5.690 (2.729-11.862)*** |
| Unfavorable | 56 (29.8) | 132 (70.2) | 1 | |||
Table 5. Factors associated with good surgical informed consent practice among the study participants in WCU-NEMMCS hospital, hosanna southern Ethiopia, 2022. N=414.
Study area and period
Study was conducted from 9 to 21 August, 2022 at WCU-NEMM comprehensive specialized Hospital, which is found in Hadiya zone Hosanna town. Hosanna is a town and separate woreda in southern Ethiopia and the administrative center of the Hadiya zone located at 230 km south west of the capital Addis Ababa in the Southern Nations, Nationalities, and People's Region (SNNPR) [14]. The hospital has a bed of 474 with an increasing capacity and renders tertiary care services to a catchment population mainly from Hadiya zone and other neighboring catchments of the partial Guraghe, Silte, Halaba and Kambata zones. It has 713 health care workers (radiologists, pharmacists, environmental health workers (nurses, midwives, doctors (including General Physicians (GPs), surgeons, gynecologists and anesthetists)) were working at surgical ward, obstetrics and gynecology ward, operating room, labor ward, Intensive Care Unit (ICU) and emergency outpatient department in the hospital. The hospital has 3 major operating rooms, which are one obstetrics and gynecology operation room/OR, one general surgery OR and one orthopedic surgery OR. Annually, on average, about 3760 patients underwent major surgical procedures including cesarean deliveries [15].
Study design
Institutional based, cross sectional study was carried out.
Study population
All health care workers who were working in WCU-NEMM comprehensive specialized hospital during the study period were the study populations.
Inclusion criteria: All health care workers who worked at least 6 months in the hospital were included.
Exclusion criteria: Health care workers, who were,
•Sick on bed and couldn’t tolerate to finish the time thatthe interview took were excluded from the study.
•Those who had not been working in surgical, labor,obstetrics and gynecology ward, operating room, ICUand emergency OPD for the last 6 months wereexcluded as they have less exposure to patients who hadundergone surgery.
Sample size determination
The sample size for proportion of SIC practice was determined by the formula for estimating single population proportion with assuming confidence interval of 95% and marginal error 5% with proportion (p= 50.1% from a previous study done in bale zone Ethiopia and non-response rate 10% (10). The formula is;
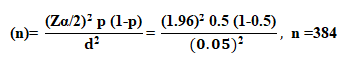
Then 10% allowance for none responding, and then the total sample size for the first objective was,
n=384+ (384 × 0.1) =384+38, n= 422.
Sampling procedure
Proportional allocation was done to get appropriate representative sample size, from the total of 630 health-care workers, including medical residence ship students (nurses, midwives, doctors, and anesthetists), found in the surgical ward, OR, emergency OPD, labor ward, obstetrics and gynecology ward, and ICU. Specifically, 334 nurse, 106 Midwives, 64 anesthetists, 76 General physicians/Gps/, 14 medical residency ship students and 36 specialist doctors, professions that work in 3 different shifts, were found in WCU-NEMM comprehensive specialized hospital. Therefore, considering regular staff rotation between each wards proportional allocation to sample size was made for each professional, then simple random sampling/SRS/ technique was used to select each participant from their respective profession [16].
Proportional allocation for each professions sample size, was done by the formula;
ni=(Ni)*(nf)/((N))
Where,
ni= Sample size for each profession.
Ni=Total number of participants in each profession.
nf= Total sample size of the study participants.
N= Total number of HCWs/source population.
| Nurse (334) | Midwifery (106) | Anesthetists (64) | General physicians (76) | Specialist (24) | Residents (14) |
|---|---|---|---|---|---|
| ni =224 | ni=71, | ni=43 | ni=51 | ni=24, | ni=09 |
Study variable
Dependent variable: Surgical informed consent practice.
Independent variables:
•Socio-demographic characteristics (age, sex, religion,work experience, language barriers).
•Organizational factors (lack of administrative support,time spent on SIC process, lack of in-service training,lack of adequate content of consent form, lack of policyor regulation in the institution, work load).
•Health care worker related factors (knowledge, attitude).
•Patient related factors (anxiety and fear of anesthesiaand surgery, cultural myths about surgery, knowledge ofSIC, influence from relatives, surgical schedules, historyof previous surgery)
Operational definitions
The practice of SIC was measured using 13 structured Likert type questions having options of “never”, “sometimes” and “always” which scored as 1, 2 and 3, respectively. The total score for practice then dichotomized into good and poor practice using the mean score 26.9976 as the cut point.
Good practice: A score greater or equal to the mean score for the practice questions.
Poor practice: A score below the mean score for the practice questions.
Knowledge of SIC was measured using 10 structured knowledge questions with multiple options, totally 13 items having “yes”, “no” and “I don’t know”. The total score for knowledge then dichotomized into good knowledge and poor knowledge using the mean score 15.615 as the cut point.
Good knowledge: A score greater or equal to the mean score for the knowledge questions.
Poor knowledge: A score below the mean score for the knowledge questions.
Attitude toward the proper SIC was measured by using 09 Likert type attitude questions. A score of 1, 2, 3, 4 and 5 was given for strongly disagree, disagree, neutral, agree and strongly agree responses, respectively. The total score for attitude then dichotomized into favorable and unfavorable attitude using the mean score 35.6 as the cut point.
Favorable attitude: A score greater or equal to the mean score for the attitude questions.
Unfavorable attitude: A score below the mean score for the attitude questions.
Health care workers: In this study, health care workers were individuals, (nurses, midwives, doctors (GPs, surgeons, gynecologists and anesthetists) those works in frontline clinical placements that are in direct contact with patients including health care students.
Major surgeries: In this study, major surgeries is defined as an operative procedure in which more extensive resection to human body is performed, like a body cavity is entered, and organ/tissue manipulation is done.
Data collection tools and techniques
Each study units were selected based on the proportionally allocated sample size from their respective profession by SRS method, then self-administered pretested questionnaire was used to collect all the necessary data on the practice and factors affecting the SIC process. The questionnaire was adapted and modified from the professional and clinical standards of the Royal College of Surgeons (RCS) of the UK, South Africa, Uganda, FMOH, and EMA and were used by Negash et al in the previous study. The questionnaire had six parts. Part I: Socio-demographic characteristics of the study participants. Part II: Organizational factors that affect practice of informed consent. Part III: Respondents knowledge of the informed consent process. Part IV: Respondents attitude toward the practice of informed consent, which contained questions with responses which ranged from strongly disagree to strongly agree. Part V: Assessed the respondents’ practice of the informed consent process, and the questions contained response options of “never”, “sometimes” and “always”. And part VI: Patient related factors that affect practice of informed consent.
Data collectors and data quality control
To ensure quality of the data, the questionnaires were translated from English in to Amharic and then back to English by bilingual professionals to maintain consistency. Pretesting was done on a limited number n=22 (5%) of similar health care professionals at Worabe compressive specializes hospital which is 60 KMs from the study area a week before actual data collection time to avoid information contamination. 3 BSc Midwifery professional data collectors and 1 MSc holder supervisor who participated to coordinate, facilitate, and supervise the overall activities, were recruited outside the study sites to avoid selection and information bias. Two days training was given to them on the objective of the study, data collection tools (how to maintain consistency and completeness of the questionnaire), and when to start data collection by the principal investigator, then the data collectors were assigned in each ward to distribute and collect back the questionnaire to and from the study participants, by revising each item of the questions, collected data was checked for completeness and clarity by the supervisor and the principal investigator.
Data processing and analysis
The collected data was checked for completeness and consistency, coded and entered into epi data version 3.1 then was exported to statistical package for social science/SPSS/ version 25 for cleaning and analysis. Data clean up was performed by checking for frequencies and missed values and variables, descriptive statistical analysis was used to show the characteristics of the participants. Binary logistic regression was used to control for confounder variables and identify factors associated with the good practice of SIC among HCWs using cut point of p-value less than 0.25, then factors with the cut point was considered as fit for multivariable analysis. The Hosmer-Lemeshow goodness of fit test was used to determine model fitness and the model was adequately fitted for the final analysis with (p-value 0.512) which was insignificant and that indicates the selected variables were important determinants. The adjusted odds ratios with their corresponding 95% confidence intervals were computed, P-values of less than 0.05 was considered significant in the final model multivariate logistic regression and the analysis result was presented as frequencies, means, standard deviations, and percentages using tables and figures.
Background
In medicine informed consent is the process of communication between a patient and health care provider that results in the patient’s authorization or agreement to undergo a specific medical/surgical intervention through Informed consent form which is a document that explains the nature and effect of the act and be given to the patients before any procedures so that they can decide to undergo the procedure or choose another option [1-3].
The central notion of informed consent is that the patients have the proposed procedure explained to them in such a way that each can decide whether he or she can proceed with the treatment. It also requires that the consent comes from the patient's own free will without coercion'. In clinical practice, the signing of a consent form, presumably should be preceded by adequate exchange of information and are only undertaken in some circumstances notably, prior to major invasive procedures such as radiologic procedures and surgery, in this respect, doctors should follow the principle of beneficence, that is, the duty of care [4].
According to the 1995 world health organization declaration on the promotion of patients rights, patients have the right to be fully informed about their health status, including the medical facts about their condition; about the proposed medical procedures, together with the potential risks and benefits of each procedure; about alternatives to the proposed procedures, including the effect of non-treatment; and about the diagnosis, prognosis and progress of treatment from the care giving health care professionals [5].
Despite this, it is inconsistently practiced and rarely achieves the theoretical ideal [6]. Some literatures states patients had poor knowledge and perception about surgical informed consent/SIC/ and the care providing professionals should provide them with the reason for operation, success of the operation, alternatives of the treatment, what would happen during the operation, for how much the operation would take, precautions after the operation and information on post treatment/post-operative/ care and free and willingness of the overall consent before consent is signed [7,8]. In Middle East (Saudi Arabia), (47%) of patients believes that saying no to what the doctors planed would mean losing their good relationship with the doctor [9]. The practice of SIC among health care providers was considered as poor and the health care workers/HCWs/ did not meet the minimum standards yet when they conducted informed consent with patients so as, it’s believed that failure to obtain adequate informed consent renders a physician liable for negligence or battery and constitutes medical malpractice. In Asia (Pakistan), most doctors think that telling patients about possible complications would discourage them from going ahead with surgery, keeping these factors in mind it is essential to formally explore the relationship of informed consent procedure with the patients' thought processes.
A limited collection of studies from the African continent reveals, SIC is provided to clients in a highly compromised manner, which includes performing surgeries immediately after obtaining clients’ signatures and without delivering any information regarding the surgical procedure to be performed, this is contrary to international recommendations, which SIC is one of the pillars of high quality care [10].
In Ethiopia, informed consent for medical procedures is a legal requirement. It was stated that medical service may not be provided without obtaining the patient’s informed consent under the Ethiopian council of minister’s regulation 299/2013, article 52.It also states, under sub-article 3, “Any health professionalshall make reasonable effort to obtain the patient’s informedconsent” [11]. The effectiveness of the informed process insatisfying the patients needs and rights and the patients' ownperception of how the process should be is an essential elementin the process of obtaining informed consent [12]. Despite ofthis, In Ethiopia, only 16.5% of surgical patients were informedabout the anesthesia to be used, types of surgery, benefits andpossible complications of the treatment from their health careproviders [13].
Therefore, this study was aimed to assess practice and factorsassociated with informed consent for major surgical proceduresamong health care workers in Wachemo university, Nigist EleniMohamed Memorial comprehensive specialized Hospital/WCU-NEMM/, Hosanna Southern Ethiopia.
Conceptual framework
The conceptual frame work shows the boundary that the study covered and the relationship which was proven after going through all the literature review. The relationship was proposed between four categories of independent variables. (Socio-demographic factors, organizational factors, patient related factors and the HCWs related factors) and the dependent variable, practice of SIC process. The relation was then depicted by one directional effect of independent variables on the dependent variables (Figure 1).
Objectives
•To determine the proportion of proper pre-operativesurgical informed consent practice for major surgicalprocedures among the health-care workers.
•To identify possible factors affecting theimplementation of proper surgical informed consentpractice among the health care workers.
AOR: Adjusted Odds Ratio; CI: Confidence Interval; CMHS: College of Medicine and Health Science; FMoH: Federal Minister of Health; ICU: Intensive Care Unit; OR: Operation Room; SIC: Surgical Informed Consent; SNNPR: Southern Nations Nationality and People’s Region; SPSS: Statistical Package for Social Science; SPHMMC: St, Paul Hospital Millennium Medical College; SRS: Simple Random Sampling
Select your language of interest to view the total content in your interested language